The mission of the National Nurse-Led Care Consortium is to advance nurse-led health care through policy, consultation, and programs to reduce health disparities and meet people’s primary care and wellness needs. Nurse-led care exists at the intersection of multidisciplinary healthcare, where nurses have a transformative role as holistic caregivers, advocates, and leaders. Nurses have unique skills and insight to treat the whole person, serving as a critical connection between compassionate and evidence-based healthcare. Nurse-led care is defined by nurses working to the full scope of their licensure as part of a team, embracing principles of nursing, to engage patients, families and communities to deliver evidence-based, whole-person care.
Guiding Principles of Nurse-Led Care
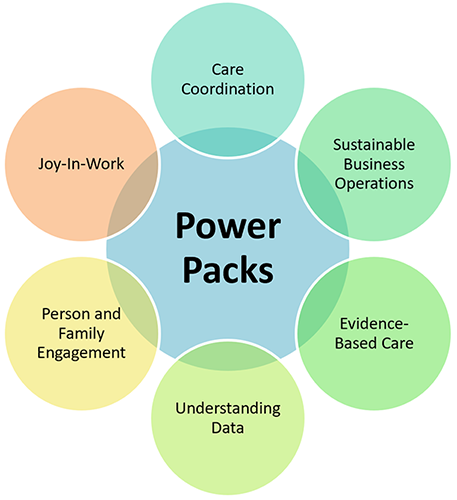
Nurse-led principles of care can be used to deliver improved outcomes for patients, staff, and the larger healthcare community. This includes:
- Commitment to nurse-leadership
- Proactive coordination of patient care
- Working as a collaborative member of the larger healthcare community
- Adoption of interdisciplinary care teams and/or adoption of care team work flows
- Integration of non-primary care services into practice
- Engagement of patients and families
- Creating a fulfilling, joyful practice experience for all staff
Nurse-Led Principles of Care in Action
Nurse Practitioner Support & Alignment Network
In 2015, NNCC and the American Association of Nurse Practitioners (AANP) partnered to create the Nurse Practitioner Support & Alignment Network (NP SAN) as part of a CMS-funded, four-year, national practice transformation initiative. As clinical practices move from fee-for-service to new, value-based payment methodologies NPs will need the skills and tools to provide patient-centered, high-quality, sustainable services. The NP SAN developed a series of workshops focused on critical principles of nurse-led care key to practice transformation. These included the optimization of interdisciplinary care teams, and the use of care teams for care coordination. NNCC conducted 18 in-person training workshops for 962 participants from 216 practices across 13 states. NP SAN training partners realized impressive improvements in patient health and cost savings as a result of their work with NNCC and the TCPI. These included:
- 8.73% reduction in uncontrolled diabetes (31,000+ lives improved)
- 2.49% increase in controlled hypertension (14,000+ lives improved)
- 2.94% reduction in emergency room visits (28,000 visits prevented)
- $162 million in cost savings to the healthcare industry due to improved health outcomes and unnecessary utilization avoided (based on estimates and claims data)
More information about the NP SAN can be found here.
Click here for Upcoming Webinars